Epidural
OP (Sunny Side Up), Cervical Swelling and Slow Dilation
OP (Sunny Side Up), Cervical Swelling and Slow Dilation…These are a few of the issues my last client had. With her permission, I want to talk about her birth. It’s actually a pretty amazing story. In addition to what I mentioned, she also had a 9lb baby with a very large head and managed to get out with only a 2nd degree tear.
So this client had been complaining of back pain for a couple of weeks. She works at a desk so I was worried that her posturing may have aided in her baby positioning himself OP (occiput posterior) or what some people call sunny side up or face up. When a baby is OP, the back of the head, which is the largest and hardest part of the head, digs into the moms back in utero. This sometimes causes chronic back pain. Some moms never feel any back pain at all when their baby is OP. I had talked with her about this and suggested that she do pelvic rocks daily and spend as much time as possible in the open knee chest position. Open knee chest is when mom puts her head and breasts on the floor and sticks her butt up in the air with her knees about hip width apart. Sounds easy but when you are very pregnant it is quite difficult. I also suggested that she sit on a birth ball that was inflated enough so that her thighs where parallel to the floor in the hopes of relaxing her pelvic floor and encouraging baby to turn. She is quite tall and I don’t think she found the ball very comfortable. I also told her no reclining on the couch. I feel as if I should have done more to encourage her to encourage the baby to turn but her back pain came and went and she didn’t feel fluttering indicating hands in the pelvic area and I couldn’t see her tummy (She was two hours away from me) to see if she had the dip in the stomach that OP babies often make. I guess I didn’t want to freak her out with all the optimal fetal positioning techniques when in reality babies that are OP before labor almost always turn before labor or in labor.
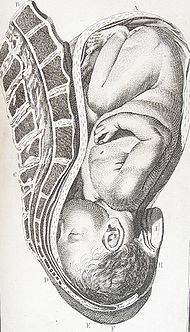
This is a baby that is occiput anterior, the optimal fetal position for easier birth…
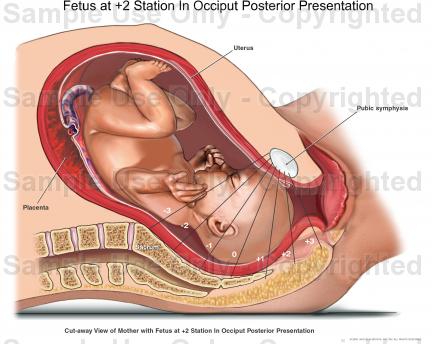
This is a picture of an occiput posterior baby. Notice how the back of the head is in the mother’s back…
This woman, who we will call Alyssa, began her labor at 4am the morning that she was 41 weeks and 3 days pregnant. At around 5am or so she began to have leaking that she believed was her water. I joined her at 9:30am. The time line for her birth m my arrival goes as follows…
9:30am: I arrive
Contractions about five minutes apart, less than one minute long
You were breathing through them very well
10:00-10:30am: We walked, contractions started getting longer and more intense
10:30-11:30am: Complaining of back pain, we do pelvic tilts and open knee chest, I worry baby is OP
Breathing well through contractions but growing more intense with each one
You rest in bed for a few contractions
11:30am: Contractions are very intense. Still around 4-5 minutes apart, a minute long.
You are ready to go to the hospital
12:00pm: We arrive at hospital. Staff is busy. We walk for half an hour and take it one contraction at a time. Back pain is intensifying and you are feeling a lot of pelvic pressure
1:00pm: You are admitted. You are 4cm and 100 effaced and your water is leaking. Baby is at a +1 station. You are monitored for half an hour and the baby looks great. You continue working through each contraction one at a time.
1:45pm: You are taken off the monitor and get into your labor room. Labor is very intense and you labor standing while leaning on the bed for an hour.
3:00pm: Labor is so intense and contractions are coming every three minutes for about a minute and a half. You have a lot of pelvic and rectal pressure. You are a bit shaky and very hot. We put ice cold towels on you.
Because labor is so intense, the nurse figures you must be very progressed and asks if you want to be checked.
You are 8cm dilated. You are having urges to push.
4:30pm: Contractions continue at 3 minutes apart and about 2 minutes long. Your back pain is much worse as is the rectal pressure. We try many positions to help complete your cervix. A check shows that you are stlil 8cm. Midwife breaks your water and your cervix closes to a 5 or 6 and the baby retreats back to a zero station. We talk about the baby possibly being OP but she cannot confirm with exam. We spend the next hour trying to get the baby to turn.
5:30pm: The nurse checks and says you are 9cm with a lip. We spend half an hour getting you in positions to aid dilation.
6:00pm: Labor has become unbearable and you are having urges to push, your back pain is very intense. Midwife checks you and you are 6cm and your cervix is swollen. She again is almost certain the baby is OP. She offers and epidural and you accept. You also have a shot of Nubain to hold you over until the epidural is placed.
7:00pm: Epidural is in place. You feel pain on one side for an hour or so.
8:30ishpm: You are 10cm
9:30ishpm: You begin pushing. The baby is at a +2/3 station when you being. After an hour is becomes clear that the baby is OP. It is also clear that he has a very large head. You push for another hour holding the squat bar and/or sheet tied to it while his head molds.
11:30pm: Baby is coming down but getting hung up on the pelvic bone. You push flat on your back with your knees pulled far back and apart. He is able to descend past the pubic bone and begins to crown. The doctor uses baby shampoo as lube and supports your perineum as you push the final few pushes before he is born.
just before
12:00am. Baby is born!!!! He comes out crying and looking around and after being checked out for a
few minutes is brought to you for skin to skin contact. You try to nurse immediately but he was interested just yet.
12:20am: Less than half an hour after being born, your baby is successfully nursing!!!
12:30am: The doctor is finished tending to you and leaves. You and dad bond with your baby.
1:30am: I leave
So the time line is a synopsis and not the birth story with all the details. What I’d like to include in that is that as her back pain intensified and the midwife agreed with me that the baby was probably OP, we began to get Alyssa into every position we could to get the baby to turn. The bed was broken down with the squat bar attached because when she was 8cm we tried to get her to sit on the bed with her legs on the lower portion with her upper body on the bar in a semi squat position in order to put pressure on the cervix to complete it. She didn’t like it because she had so much rectal pressure, so we took the bar off but left the bed broken down. Once the OP presentation because very obvious, we had her lower body on the bottom part of the bed with her upper body on the middle so that she was basically on her hands and knees. We tried to apply counter pressure but Alyssa didn’t like it. She had not wanted very much massage or touch so we didn’t not try to relieve her back pain that way. She mostly responded to cold on her lower back.
Another point I’d like to talk about is that she was at 8cm for more than two hours before the midwife broke her water. She had been in active labor for about 13 hours at that point and was ready for things to move along. By this point her labor had become all but unbearable. I believe that the baby’s OP presentation was making labor much much more painful. She was already beginning to lose control during and even between contractions and I think that even though AROM (artificial rupture of membranes) was not part of her birth plan, it really did sound like the best idea at the time. Of course, once it was done and the midwife felt her cervix close and the baby retract, she had this “OH SH!T” look on her face. And also of course, once it was done the contractions became even more intense.
I am not sure if the midwife breaking the water at 8cm is what caused the chain of events that followed. If it would have broken on it’s own, the same thing could have happen. I had it happen with another OP baby client. Her bag ruptured spontaneously at 8cm and her cervix went back down to 7cm and the baby retracted from +1 to -1/0 station. I also think that after having been at 8cm for two hours with transition strength contractions after having labored all day, that Alyssa was running out of both steam and motivation, understandably.
The former OP client I mentioned who went from 8cm to 7cm took SIX FULL HOURS to get from 8cm to complete. She had no option for an epidural as she was in a Korean hospital that did not offer them outside of business hours. The doctor was also performing c section so she didn’t have anyone offering to end the labor for her and her cervix wasn’t swelling either. She managed and made it through it but it was incredibly difficult. I have no doubt that in that scenario that Alyssa could have continued her labor without an epidural.
What made Alyssa’s labor even more difficult was to spend two hours at 8cm with pushing urges, eventually get told she was 9cm and still have pushing urges and then learn that she was 6cm with a swollen cervix. I think that hearing this was incredibly difficult for her. Maybe there were too many vaginal exams, maybe she didn’t have to know all of that was going on with her cervix but the fact is, she was pushing involuntarily even at only 6cm.
I have read that premature pushing does not always make a cervix swell and that her swelling was probably more the result of fetal positioning. It could also be a combination of the two, it’s hard to say. At any rate, with the intensity of pain she was feeling the midwife thought it best that Alyssa get an epidural to relax enough to be able to dilate. I was incredibly worried about this because it would be hard to get the baby to rotate with the epidural but I really do believe that at this point it was necessary. Her cervix wasn’t going to get a break and she was in too much pain to be able to invert her with open knee chest to pack the baby out of the pelvis some.
The midwife was right, the epidural helped and she dilated quickly. As the time line mentions, she pushed for nearly two and a half hours. The head was large and had a lot of molding at birth. He did get hung up under the pubic bone but the McRoberts maneuver, flat on back, knees far apart and up as possible dislodged him and within a few pushes he was out.
The most amazing part of this birth is that mom had only a second degree tear. OP babies are often associated with a higher incident of third and forth degree perineal tears and considering the size of this baby as well, I think this mom was incredibly lucky. I think that the fact that Alyssa had a successful vaginal delivery is a little bit of a miracle. We had THE BEST nurse on staff that day who helped me encourage Alyssa to move through her labor before she got the epidural. We had her doing a lot of things she didn’t want to do but she trusted us and we helped her and she did it. All of these things helped, I really believe this. They helped her baby move down so that when she did get the epidural, labor continued to progress. The support continued after the epidural in that we continued to help her move to help the baby move down. The woman used a squat bar to push with an epidural, THAT is a feat in and of itself. It took three of us (nurse, dad, me) to support her through it but she totally did it.
Here are some facts that I found regarding OP babies…
- The incidence of persistent occiput posterior babies at delivery is about 5.5% overall
- With a persistent posterior, both first and second stages are prolonged (Ponkey et al). However, longer second stages do not in themselves cause worse maternal or neonatal outcomes; in one study, as long as the fetus was stable, the second stage could continue without harm to mother or baby (Kuo et al).
- The likelihood of cesarean section or instrumental delivery (forceps or vacuum extractor) is greater when there is a persistent posterior position; in fact, the 5.5% of persistent posteriors account for 12% of all cesarean deliveries performed for dystocia (Fitzpatrick et al).
- Persistent posterior positions are associated with an increased incidence of premature rupture of the membranes, oxytocin induction and augmentation, epidural analgesia, chorioamnionitis, , episiotomies, severe perineal lacerations, vaginal lacerations, excessive blood loss, and postpartum infection (Pearl et al, Ponkey et al).
- Worse, there is a sevenfold increase in the incidence of anal sphincter injury, that is, third- or fourth-degree perineal lacerations (Fitzpatrick et al). Babies delivered from the posterior position were more likely to have Erb’s Palsy and facial nerve palsy than those delivered from the anterior position (Pearl et al)
- Occiput posterior babies often times cause a premature urge to push (pushing before 10 cm dilated)
- Occiput posterior babies can cause cervical swelling due to the hardest part of the head bearing down unevenly on the cervix. Cervical swelling can cause a stall in dilation or not allow the baby to descend enough to be pushed out despite the mother’s best efforts.
This study also explains the implications of epidurals with OP babies…
Epidural Analgesia Linked to Increased Risk of Occiput- Posterior Babies
Lieberman, E., Davidson, K., Lee-Parritz, A., & Shearer, E. (2005). Changes in fetal position during labor and their association with epidural analgesia. Obstetrics & Gynecology, 105 (5, Part 1), 974-982. [Abstract]
Summary: This prospective cohort study used periodic ultrasound examinations during labor to evaluate changes in fetal position and their relationship with epidural analgesia. The researchers sought to determine whether epidural analgesia is responsible for higher rates of fetal malposition (occiput-posterior (OP) or occiput transverse (OT)) or whether women experiencing labor with a malpositioned baby have more painful labors and are therefore more likely to request epidural pain relief. A total of 1562 nulliparous, low-risk pregnant women were enrolled in the study.The researchers found that the position of the baby (occiput anterior (OA), OP or OT) at the time of enrollment (in the early part of active labor) predicted position at birth poorly. For instance, of the women with an OP baby at birth, only 31% had a baby in the OP position at the initial ultrasound scan. Similarly, sonograms done later in labor were also poor predictors of position at birth. The data demonstrated that changes in fetal position were common during labor, with 36% of participants having an OP baby at the time of at least one scan. More than one-half of the women who gave birth to a baby in the OP position never had an OP baby at any ultrasound assessment in labor. Overall, 79.8% of babies were born in the OA position, 8.1% were OT, and 12.2% were OP at birth.Epidural analgesia was strongly associated with delivery from the OP position: 12.9% of women with epidurals gave birth to babies in the OP position versus 3.3% of women without epidurals (relative risk 4.0, 95% CI 1.5-10.5). Transverse position was not related to epidural use. In a statistical model that controlled for various medical and obstetric factors that could affect outcomes, epidural use was still associated with a 4-fold increase in the risk of OP birth.
The data suggest that the association between epidurals and OP babies is not because women in labor with an OP baby are more likely to request an epidural. Women who received epidurals were no more likely to have OP babies at prior to or at the time that the epidural was administered. Furthermore, women with OP babies in labor or at birth reported the same degree of pain as those with OA or OT babies and were no more likely to report “back labor,” which is commonly thought to be related to the OP position. Finally, women with OP or OT babies at birth were much more likely that those with babies in the OA position to give birth by cesarean section, with 6.3% of OA babies born by c-section versus 64.7% of OP and 73.8% of OT babies (p<.001).
Significance for Normal Birth: Epidural use increases the risk of instrumental (forceps or vacuum) delivery in first-time mothers. Experts have proposed various reasons for this association, including diminished urge to push and changes in the tone of the pelvic floor muscles that inhibit proper rotation of the fetal head. Letting the epidural “wear off” has been thought to increase the likelihood of unassisted vaginal birth, however, this systematic review calls into question that common practice.
In normal birth, there are complex hormonal shifts that help labor progress and facilitate delivery. The laboring woman produces natural endorphins that help her manage the pain of labor. Her ability to move freely and assume a variety of positions while pushing work in concert with these hormonal changes. Epidural analgesia numbs the sensations of birth, and the production of natural endorphins ceases as a result of the disruption of the hormonal feedback system. When the epidural is discontinued, the woman’s pain returns but her natural endorphins may remain diminished and therefore her pain may be greater than if the epidural had not been given in the first place. Furthermore, when an epidural is administered, the woman is usually confined to bed and attached to fetal monitors and an intravenous line. The woman and provider may become accustomed to laboring in the bed attached to machines. When the epidural is discontinued the restrictions! on her movement may persist. Under these conditions, it is likely that the impact of an epidural on normal birth may outlast the epidural itself.Ann Tumblin also sent me this regarding OP (face up) babies. It was done by Penny Simkin who is basically the mother of all doulas. It is very informative so if you have ever had an OP baby and are nervous about it a second time, I highly recommend you taking a look at it.
I believe that Alyssa’s birth outcome was the combination of her determination and trust that we were supporting her in every way we could and we were. I was sore the next morning which isn’t saying much compared to how she felt but more of a testament to the work I was doing. We were incredibly lucky to have the staff that we had and I also believe that if any piece of the puzzle had of been missing that her birth story would be very different. I think the point that I want to make about her birth is that if a mother is supported completely and if epidurals are not done too early that even very difficult births can have a great outcome. Mom is satisfied with her experience which is, other than healthy baby and mom, the best thing.
If you had an OP baby, please share your experience with us.
Read Full Post | Make a Comment ( 39 so far )The Six Care Practices that Support Normal Birth (Part Three)
In Part One and Part Two of this segment, I discussed why I believe in the six care practices and the first three of the care practices which include: labor begins on its own , freedom of movement throughout labor and continuous labor support. The six care practices that support normal birth are based on research and evidence based maternity care. This is the healthiest and safest way to have a baby in most cases. In a normal healthy pregnancy most women can and should deliver their babies vaginally and with few interventions. All this medicalization of labor and delivery is not only not necessary, it’s also causes problems.
The fourth care practice is no routine interventions.
Routine interventions are anything that is done or not allowed at hospital that isn’t medically necessary. Evidence based maternity care through research has shown that these interventions are not only not necessary but can cause more harm than good when used routinely. Here is a list of the most common routine interventions.
Restriction on eating and drinking: Back in the day when women were knocked out with general anesthesia food and drink were not allowed in case the woman vomited and inhaled it. Rarely is general ever used any more but it’s still the policy at most hospitals. Women need food and drink to keep their bodies fueled and hydrated for the hard work of labor.
Use of IV fluids: Because of the restriction on drink, the IV fluids are given to keep the mom from getting dehydrated. IV fluids are just not properly balanced in a way that gives the mom the energy she needs to labor. The intervention spiral tends to begin with the IV and it’s easy access to the vein and it also keeps you tethered and restricts movement. The IV line does provide quick access to the vein in case of an emergency. One compromise is a heparin lock. It’s the little catheter that put in the vein and shut off without the IV line actually being connected.
Continuous electronic fetal monitoring: In a normal low risk labor continuous EFM isn’t recommended. Intermittent monitoring, or 20 minutes out of every hour is just as beneficial. With intermittent monitoring the mom is allowed the freedom of movement. Continuous EFM increases the number of inventions without improving outcomes.
Speeding up labor: Artificial rupture of membranes and augmentation of labor: Speeding up labor sounds pretty tempting but when the water is artifically ruptured (AROM) it increases the pain of the labor and removes the baby’s cusion to move around and get into a better position. Infection risks are increased and most hospitals have a time limit on how long the water can be broken before intervening. Augmenting labor with pitocin can make labor go faster but it also interupts the normal flow of hormones and makes labor much more painful while increasing the risk of fetal distress.
Epidurals: Epidurals do take the pain away (most times) but can also cause a cascade of other interventions and problems. They increase the risk of an OP baby (sunny side up) because the pelvis is over relaxed and baby finds it harder to rotate and turn without the gravity because mom is stuck in bed. The risk of c section increases and the drugs do reach the baby potentially causing breastfeeding problems. Please see my post To Epidural or Not to Epidural for more details on the risks of epidurals. There are many other ways to cope with labor. Preparing physically and mentally for labor, continuous labor support and avoiding routine interventions all help make labor an easier process.
Episiotomy: Routine episiotomy can be more harmful than tearing. Tears typically aren’t as bad as the cut would be and they heal faster. Episiotomy frequently causes more tearing and more pain. Avoiding epidurals and upright pushing positions reduce the risk of or need for episiotomy.
Medical need for interventions are occasionally necessary. Routine intervention should be avoided. Learning about the routine interventions and when they may become necessary and writing a birth plan can help reduce the chance of having routine interventions forced on a laboring woman. I think it is also very important for the partner to understand these procedures so that they can assist the mother as much as possible. Research is on the side of the mother when it comes to these routine interventions and discussing the written birth plan before the birth will help the labor go more smoothly. Hiring a doula can also help keep routine interventions from being carried out as she can remind the mom of what the risks and benefits of the interventions are and of what her wants are.
Read Full Post | Make a Comment ( 5 so far )Going “Natural” and Being a “Hero”
It makes me so mad when I hear women say “I am not one of those women who think I have to prove something and not get drugs.” Are they just trying to justify themselves with that? Do they think they have to defend their decision to use drugs in their birth? I have never had a client come to me and that she wants to go natural and the reasons for it are bragging rights. Quite frankly, I would rather hear the woman that says she thinks she is too wimpy to do it without an epidural. Then I can tell her how wrong she is and that she is completely capable of birthing her baby without an epidural because I have never met a woman that I thought couldn’t do it, that every woman has the strength and ability to do and that yes she may need help but she can totally and completely do it! I would tell her about a client of mine that is a girly girl and self admitted wimp that naturally birthed an OP baby after a HARD 36 hour labor and how she was happier with that birth experience than with her first epiduralized birth that included 25 hours of pitocin, 50 stitches from an episiotomy, a vaccum assisted birth, and a baby with meconium aspiration that spent 10 days in the NICU.
And while we are on it, going natural does not mean not having a c section. It means not using drugs or interventions although if you tell a couple of my med free moms that because they got an IV line they don’t count as having had a natural birth they might smack you for it. But really, if you are having a completely natural birth, you are not medicating, having an IV line, having an episiotomy or having any other routine intervention. You are just having your baby. If you are not having a c section then you are having a vaginal birth. It’s ok to say vagina or vaginal or vaginally. Really, it is.
But back to the whole hero thing…it just drives me nuts when I hear the whole “I don’t have to be a hero in the delivery room” bit. It has absolutely nothing to do with being a hero or with what anyone else thinks. Moms that come to me that want my help in having a natural birth do it because it is safer and healthier for both the mom and the baby. They want the natural experience of birthing their child with their body. They want to give their baby a gentle start without drugs in their systems. They want to minimize the risks of forceps and vacuum and cesareans. They want to minimize the risks of tearing because they have the ability to feel what is happening as it happens. They want to move during their labor and not be forced to push on their back. They want to reduce the risks of breastfeeding issues because having an epidural can cause latch problems for the baby. They do not want to run the risk of having pitocin because the epidural over relaxed their uteri. They understand that by having drugs they increase the risk of fetal distress and c section. They could care less about being a hero in the delivery room. I doubt any of them ever even had that thought.
Read Full Post | Make a Comment ( 12 so far )To Epidural or Not to Epidural
That is the question that many moms automatically say yes to, no other questions asked. Now, you may think that because I am a doula that I am anti-epidural, pro natural birth only. That is true and not true all at the same time. I am pro natural birth but do realize there are some times when the epidural is more beneficial to the mother than the risks it creates for both mom and baby. I have not had a client get an epidural yet but I would totally support her if she did. Even if she were a planned epidural. I believe all laboring women need support regardless of how they labor. But that’s not really what this post is about. I just wanted to get all that out of the way first so that no one thinks that I am judging. I am not judging and I will try to be as factual as possible. Personally, I am anti-epidural for myself. For everyone else, I say do what you need to do, just make sure you have all the information you need to make the best decision possible. That’s what I am attempting here.
So, why is it that so many women say they want the epidural before they ever even have their first contraction? My bet is fear. We fear birth. Our culture fears birth. We are taught that child birth will be the most excruciating pain we will ever experience. That may be true but it doesn’t mean we can’t handle it. We can SO handle it. We were made to handle it. Here’s a really nice video made by someone researching fear in childbirth…
There are just things that we need to be able to handle child birth that are often times denied to laboring women.
What do laboring women need?
Love
Support
Encouragement
Food
Water
Movement
Touch
Safety
Peace
Quiet
Comfort
Anyone who has ever had a baby in a hospital knows that some of those things are very hard to come by. So instead, we end up being afraid and in more pain that would be otherwise. For every positive birth experience, we hear 10 horrifying ones. No wonder we run straight to epidurals! But what do we know about epidurals? How much do we understand? Do they really make birth better? The video said that people do not report a higher satisfaction with their birth because they got one. I have a client who had one her first birth and didn’t have one the second time and she was way more satisfied the second time. It’s been six weeks and she’s STILL glowing about her natural birth and how much easier recovery was. Why is this?
SO what exactly is an epidural? Here is the Wiki definition. Here is a video showing how they are administered…
How an Epidural is Administered
What kind of drugs are in an epidural?
A epidural typically has a combination of local anesthetics and opioids. This combination works better than either type of drug used alone. Common local anesthetics include lidocaine, bupivacaine, ropivacaine, and chloroprocaine. Common opioids include morphine, fentanyl, sufentanil, and pethidine (known as meperidine in the U.S.).
What does an epidural do to the baby? According to the American Pregnancy Association:
How can an epidural affect my baby? As stated above, research on the effects of epidurals on newborn health is somewhat ambiguous and many factors may be contributing to newborn health at the time of birth. How much of an effect these medications will have is difficult to judge and could vary based on dosage, how long labor continues and individual babies. Dosages and medications vary, so concrete information from research is lacking. Studies reveal that some babies may initially have trouble “latching on” among other difficulties with breastfeeding. While in-utero, they may become lethargic and have trouble getting into position for delivery. These medications have been known to cause respiratory depression, and decreased fetal heart rate in newborns. Though the medication may not harm the baby, the baby may experience subtle effects like those mentioned above.
That answer is kind of unclear so I looked around for some more answers. This doctor from New Zealand says:
There is a noticeable lack of research and information about the effects of epidurals on babies. Drugs used in epidurals can reach levels at least as high as those in the mother25, and because of the baby’s immature liver, these drugs take a long time- sometimes days- to be cleared from the baby’s body26. Although findings are not consistent, possible problems, such as rapid breathing in the first few hours27 and vulnerability to low blood sugar28 suggest that these drugs have measurable effects on the newborn baby.
Several studies have found subtle but definite changes in the behavior of newborn babies after epidural36 37 38 with one study showing that behavioral abnormalities persisted for at least six weeks39. Other studies have shown that, after an epidural, mothers spent less time with their newborn babies40, and described their babies at one month as more difficult to care for41.
While an epidural is certainly the most effective form of pain relief available, it is worth considering that ultimate satisfaction with the experience of giving birth may not be related to lack of pain. In fact, a UK survey which asked about satisfaction a year after the birth found that despite having the lowest self-rating for pain in labor (29 points out of 100), women who had given birth with an epidural were the most likely to be dissatisfied with their experience a year later42.
(please go here for the references).
What are the risks to the mom?
Here is a link to Ronnie Falcao’s website, www.gentlebirth.org. She has TONS of information on all sorts of topics posted by midwives all over the country. I chose this page to discuss epidural risk to moms because this link has many midwives weighing in on it rather than just one source. Here are what some of them had to say…
The incidence of chronic back pain (lasting weeks to months) is reported at 10-15%.
Episodes of hypotension are quite frequent in my experience, despite IV fluid loading prior to the procedure. These frequently cause fetal bradycardias and all the resulting interventions, chaos, and fear.
Late decelerations (usually with good variability and referred to as “reflex lates”) are a common sequelae of epidurals. They are not threatening in and of themselves, but they create a cascade of intervention.
Fever is not uncommon (about 20-25%, I believe) and can cause many interventions for mom and baby.
Spinal headaches are unusual in skilled hands, but I’ve seen them.
Vacuum and forceps delivery are significantly increased, as is cesarean section if the epidural is given before 4-5 cm.
Here is what the American Pregnancy Association says of maternal risks of epidural use…
* Epidurals may cause your blood pressure to suddenly drop. For this reason your blood pressure will be routinely checked to make sure there is adequate blood flow to your baby. If this happens you may need to be treated with IV fluids, medications, and oxygen
* You may experience a severe headache caused by leakage of spinal fluid. Less than 1% of women experience this side effect from epidural use. If symptoms persist, a special procedure called a “blood patch”, an injection of your blood into the epidural space, can be done to relieve the headache
* After your epidural is placed, you will need to alternate from lying on one side to the other in bed and have continuous monitoring for changes in fetal heart rate. Lying in one position can sometimes cause labor to slow down or stop
* You may experience the following side effects: shivering, ringing of the ears, backache, soreness where the needle is inserted, nausea, or difficulty urinating
* You may find that your epidural makes pushing more difficult and additional interventions such as Pitocin, forceps, vacuum extraction or cesarean may become necessary
* For a few hours after birth the lower half of your body may feel numb which will require you to walk with assistance
* In rare instances, permanent nerve damage may result in the area where the catheter was inserted.
* Though research is somewhat ambiguous, most studies suggest some babies will have trouble “latching on” which can lead to breastfeeding difficulties. Other studies suggest that the baby may experience respiratory depression, fetal malpositioning; and an increase in fetal heart rate variability, which may increase the need for forceps, vacuum, cesarean deliveries and episiotomies.
Epidural use is also associated with positioning problems during labor. Please see my post on Optimal Fetal Positioning for more details.
So there are some risks to both baby and mom. What are the benefits?
The first one I can think of is pain relief. The APA lists their benefits as:
* Allows you to rest if your labor is prolonged
* Relieving the discomfort of childbirth can help some woman have a more positive birth experience
* Most of the time an epidural will allow you to remain alert and be an active participant in your birth
* If you deliver by cesarean, an epidural anesthesia will allow you to stay awake and also provide effective pain relief during recovery
* When other types of coping mechanisms are not helping any longer, an epidural may be what you need to move through exhaustion, irritability, and fatigue. An epidural may allow you to rest, relax, get focused and give you the strength to move forward as an active participant in your birth experience.
* The use of epidural anesthesia during childbirth is continually being perfected and much of its success depends on the care in which it is administered.
To be honest, I think there are some crappy benefits on that list. Why are we talking c section alertness if we are talking about an epidural being used in a vaginal delivery? And “The use of epidural anesthesia during childbirth is continually being perfected and much of its success depends on the care in which it is administered.” is not a benefit of an epidural, that is a justification for screw ups.
Let’s be honest though, there are occasionally moms who really do benefit from them. If a mom is hysterical and tense and not coping at all and stalled at 5cm, she may need an epidural to relax enough to dilate. I have never had that happen with a client but have had other doulas tell me stories of it. I am not versed on the medical reasons to have an epidural but I have heard of moms being given them because their blood pressure was dangerously high and the epidural would bring it down.
I know, childbirth is HARD. It can be incredibly difficult for some women while other women do it like they do it every day. My husband’s great grandmother had 14 home births in rural Alabama during the first half of the 1900’s. They are still alive today but one, by the way. It can be painful. Extremely painful for some people but then there are those who have almost pain free labors. The thing about labor pain is that it has a purpose. As humans we are conditioned to respond to pain with fear for our own safety. Labor pain, unlike other pain, is actually doing something, it has a purpose. If we are supported in a way that allows us and reminds us of this and that our body is kindly giving us a break in between those contractions, we can take them one at a time and do it! For some of us, labor last days even. It’s usually not hard work for all of those days though. It’s not something we can’t handle.
Getting an epidural is completely a personal choice. I truly believe that we all have the ability to birth without one if we are provided with everything we need to do it. In fact, I have never met a woman yet that I thought “now SHE will totally need an epidural, she can’t do this.” If we have loving support and encouragement and all of the other needs I listed earlier, we CAN birth our babies. We have to learn to trust birth rather than fear it. We have to learn that it is a process and that interfering with the process causes more harm than good. We have to learn to prepare our bodies and our minds for delivery. We have to learn our options. I hope that in this post I have shed some light on the risks of epidural use. I hope that I can inspire some of you to go from here and learn more.
Read Full Post | Make a Comment ( 19 so far )
