breech
Breech Pregnancy and Birth Survey
All North American women who have had breech pregnancies or births are invited participate in an essay-response survey, which takes approximately 15-30 minutes to complete. We are interested in participants who had breech pregnancies (breech babies who turned head-down before birth). We would also like to hear from women who have given birth to breech babies, whether vaginally or by cesarean section; with midwives, physicians, or unassisted; at home, in a birth center or in a hospital. We welcome input from both singleton and multiple (twin, triplet, etc) breech pregnancies and births.
How to Participate:
To take the survey, please visit the Breech Pregnancy and Birth Survey
.
Read Full Post | Make a Comment ( 8 so far )Optimal Fetal Positioning for a Better Birth
‘Optimal Fetal Positioning‘ (OFP) is a theory developed by a midwife, Jean Sutton, and Pauline Scott, an antenatal teacher, who found that the mother’s position and movement could influence the way her baby lay in the womb in the final weeks of pregnancy. Many difficult labors result from ‘malpresentation’, where the baby’s position makes it hard for the head to move through the pelvis, so changing the way the baby lies could make birth easier for mother and child.
This is near and dear to my heart and something that I tend to go into depth with my clients on. It is SO SO SO very important and it is rarely discussed in prenatal visits with OBs. It’s not really something discussed at prenatal visits with OBs amd I’m assuming that it’s because positioning doesn’t really matter when the baby can be cut out if it’s a problem. Midwives and my homebirth OB in Korea as well as other natural minded OBs tend to spend more time on this. Anyway, it’s near and dear to my heart because I had a difficult position with my first baby, face first. Face first and face up or occiput posterior, OP, are two different presentations. Face first is rare, one in 500 at most. It is a position that is refrequently sectioned because the labor is very slow but it is vaginally deliverable in some situations. It is very uncommon and there are reported cases of broken necks and facial paralysis but I think that is generally due to pitocin augmentation causing much stronger contractions that the face first baby can handle. I planned a natural birth and after three days of contractions, meconium and fetal distress was sectioned (for failure to progress) only to find a face first presentation that ultimately resulted in an inverted T incision (which I will discuss in depth in another post).
The first picture is a face first presentation. The second is the optimal occiput anterior presentation.

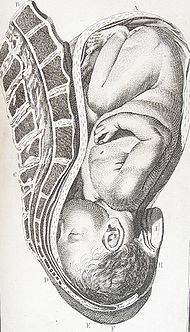
I am also including the chart below that shows the presentation view from the outlet. My son was Face First, LMT, left mentum transverse. This is considered to be a physically impossible presentation for vaginal delivery and the occurrence is extremely rare.

I spent a TON of time talking and reading and researching what happened, what caused this and how it could have been prevented and there are many things that I did wrong. I have healed from all of this and am completely capable of talking about it as I think that everyone should know how they can affect their labor, by the way. My situation was a series of events. First, poor diet in early pregnancy led to early swelling. Pitting edema at fifteen weeks usually raises red flags and of course I was told to sit with my feet elevated above my hips as much as possible, which of course I did (I mean who doesn’t want to be lazy when pregnant???). I continued with my poor diet and now lack of exercise throughout the pregnancy and managed to gain 60lbs. Sitting in a reclined position is the worst thing you can do in pregnancy because it causes the pelvis floor to tighten and the uterus to tilt so the baby has to find a comfortable position somehow and mine settled ROT (right occiput transverse, right side of my stomach, back of the head towards my back and sideways, you would see the babes profile). This apparently is the best position for a baby to flip OP (occiput posterior, face up) during labor. Instead of doing that, mine just stuck his face in my pelvis. This causes a hyperextended neck and really, faces don’t dilate cervixes.
There are a number of things that I could have done differently but I’ll get to that in a bit. First I want to discuss what the optimal position is. Then I’ll tell you how to get there.
The ‘occiput anterior‘ position is ideal for birth – it means that the baby is lined up so as to fit through your pelvis as easily as possible. The baby is head down, facing your back, with his back on one side of the front of your tummy. In this position, the baby’s head is easily ‘flexed’, ie his chin tucked onto his chest, so that the smallest part of his head will be applied to the cervix first. The diameter of his head which has to fit through the pelvis is approximately 9.5 cm, and the circumference approximately 27.5cm. The position is usually ‘Left Occiput Anterior’ or LOA – occasionally the baby may be Right Occiput Anterior or ROA.
Gail Tully, creater of http://www.spinningbabies.com
is a midwife who is very knowledgable in OFP and who helped me understand my situation better, created this to help explain positioning:

SO, how to achieve optimal fetal positioning? Very simply actually. First, posture. Gail Tully and Jean Sutton say no furniture! Sit indian style in the floor, this helps open your pelvis and release your pelvic floor. Use a birth ball for better posture. “Rest Smart” Nap or sleep in positions that let your baby’s back settle in your “hammock.”
To help facilitate good positioning, pelvic tilts should be done daily and several times a day. Walking and prenatal yoga also help with positioning by moving your hips and pelvis, stretching things out and encouraging the baby to engage in an occiput anterior position. Remember though, HEAD DOWN IS NOT ENOUGH! Babies can be head down but OP (face up) or asynclitic which can cause really long hard back labors. Read here to learn more.
So you may need to figure out what position your baby is in to begin with. Belly Mapping can help with that. By feeling where the baby is, where you feel movement, where the heart beat is, the shape of moms tummy, we can figure out how the baby is positioned. It isn’t hard to do at all. Once you learn the postition, you can then focus on improving it or changing it completely. Sometimes we know before labor even starts that the baby is OP and can get the baby to rotate. There are also ways to get a breech baby to turn.
Every pregnant woman should know this information. It is so vital in ensuring that you have the best labor and delivery possible. Sometimes breech babies won’t turn and sometimes OP babies stay OP but by learning OFP techniques you are at least giving yourself a chance to make a difference.
If you are pregnant here’s a list to help with positioning:
Pelvic tilts 20 each 3x per day
Sit indian style
Do not recline
Use a birth ball
Take at least a 20 minute walk every day
Learn what position your baby is in now
Learn what to do to improve the position
Learn what to do to keep the baby in that position
Get help if you are unsure
Get help if the baby won’t move
Good luck!
EDIT: Here is some information sent to me by Ann Tumblin concerning OP babies and epidural use.
Epidural Analgesia Linked to Increased Risk of Occiput- Posterior Babies
Lieberman, E., Davidson, K., Lee-Parritz, A., & Shearer, E. (2005). Changes in fetal position during labor and their association with epidural analgesia. Obstetrics & Gynecology, 105 (5, Part 1), 974-982. [Abstract]
Summary: This prospective cohort study used periodic ultrasound examinations during labor to evaluate changes in fetal position and their relationship with epidural analgesia. The researchers sought to determine whether epidural analgesia is responsible for higher rates of fetal malposition (occiput-posterior (OP) or occiput transverse (OT)) or whether women experiencing labor with a malpositioned baby have more painful labors and are therefore more likely to request epidural pain relief. A total of 1562 nulliparous, low-risk pregnant women were enrolled in the study.
The researchers found that the position of the baby (occiput anterior (OA), OP or OT) at the time of enrollment (in the early part of active labor) predicted position at birth poorly. For instance, of the women with an OP baby at birth, only 31% had a baby in the OP position at the initial ultrasound scan. Similarly, sonograms done later in labor were also poor predictors of position at birth. The data demonstrated that changes in fetal position were common during labor, with 36% of participants having an OP baby at the time of at least one scan. More than one-half of the women who gave birth to a baby in the OP position never had an OP baby at any ultrasound assessment in labor. Overall, 79.8% of babies were born in the OA position, 8.1% were OT, and 12.2% were OP at birth.
Epidural analgesia was strongly associated with delivery from the OP position: 12.9% of women with epidurals gave birth to babies in the OP position versus 3.3% of women without epidurals (relative risk 4.0, 95% CI 1.5-10.5). Transverse position was not related to epidural use. In a statistical model that controlled for various medical and obstetric factors that could affect outcomes, epidural use was still associated with a 4-fold increase in the risk of OP birth.
The data suggest that the association between epidurals and OP babies is not because women in labor with an OP baby are more likely to request an epidural. Women who received epidurals were no more likely to have OP babies at prior to or at the time that the epidural was administered. Furthermore, women with OP babies in labor or at birth reported the same degree of pain as those with OA or OT babies and were no more likely to report “back labor,” which is commonly thought to be related to the OP position. Finally, women with OP or OT babies at birth were much more likely that those with babies in the OA position to give birth by cesarean section, with 6.3% of OA babies born by c-section versus 64.7% of OP and 73.8% of OT babies (p<.001).
Significance for Normal Birth: Epidural use increases the risk of instrumental (forceps or vacuum) delivery in first-time mothers. Experts have proposed various reasons for this association, including diminished urge to push and changes in the tone of the pelvic floor muscles that inhibit proper rotation of the fetal head. Letting the epidural “wear off” has been thought to increase the likelihood of unassisted vaginal birth, however, this systematic review calls into question that common practice.
In normal birth, there are complex hormonal shifts that help labor progress and facilitate delivery. The laboring woman produces natural endorphins that help her manage the pain of labor. Her ability to move freely and assume a variety of positions while pushing work in concert with these hormonal changes. Epidural analgesia numbs the sensations of birth, and the production of natural endorphins ceases as a result of the disruption of the hormonal feedback system. When the epidural is discontinued, the woman’s pain returns but her natural endorphins may remain diminished and therefore her pain may be greater than if the epidural had not been given in the first place. Furthermore, when an epidural is administered, the woman is usually confined to bed and attached to fetal monitors and an intravenous line. The woman and provider may become accustomed to laboring in the bed attached to machines. When the epidural is discontinued the restrictions! on her movement may persist. Under these conditions, it is likely that the impact of an epidural on normal birth may outlast the epidural itself.
EDIT: Ann Tumblin also sent me this regarding OP (face up) babies. It was done by Penny Simkin who is basically the mother of all doulas. It is very informative so if you have ever had an OP baby and are nervous about it a second time, I highly recommend you taking a look at it.
Read Full Post | Make a Comment ( 48 so far )
