Optimal Fetal Positioning for a Better Birth
‘Optimal Fetal Positioning‘ (OFP) is a theory developed by a midwife, Jean Sutton, and Pauline Scott, an antenatal teacher, who found that the mother’s position and movement could influence the way her baby lay in the womb in the final weeks of pregnancy. Many difficult labors result from ‘malpresentation’, where the baby’s position makes it hard for the head to move through the pelvis, so changing the way the baby lies could make birth easier for mother and child.
This is near and dear to my heart and something that I tend to go into depth with my clients on. It is SO SO SO very important and it is rarely discussed in prenatal visits with OBs. It’s not really something discussed at prenatal visits with OBs amd I’m assuming that it’s because positioning doesn’t really matter when the baby can be cut out if it’s a problem. Midwives and my homebirth OB in Korea as well as other natural minded OBs tend to spend more time on this. Anyway, it’s near and dear to my heart because I had a difficult position with my first baby, face first. Face first and face up or occiput posterior, OP, are two different presentations. Face first is rare, one in 500 at most. It is a position that is refrequently sectioned because the labor is very slow but it is vaginally deliverable in some situations. It is very uncommon and there are reported cases of broken necks and facial paralysis but I think that is generally due to pitocin augmentation causing much stronger contractions that the face first baby can handle. I planned a natural birth and after three days of contractions, meconium and fetal distress was sectioned (for failure to progress) only to find a face first presentation that ultimately resulted in an inverted T incision (which I will discuss in depth in another post).
The first picture is a face first presentation. The second is the optimal occiput anterior presentation.

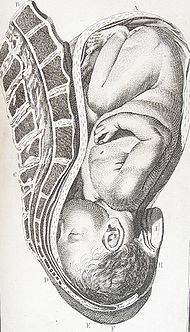
I am also including the chart below that shows the presentation view from the outlet. My son was Face First, LMT, left mentum transverse. This is considered to be a physically impossible presentation for vaginal delivery and the occurrence is extremely rare.

I spent a TON of time talking and reading and researching what happened, what caused this and how it could have been prevented and there are many things that I did wrong. I have healed from all of this and am completely capable of talking about it as I think that everyone should know how they can affect their labor, by the way. My situation was a series of events. First, poor diet in early pregnancy led to early swelling. Pitting edema at fifteen weeks usually raises red flags and of course I was told to sit with my feet elevated above my hips as much as possible, which of course I did (I mean who doesn’t want to be lazy when pregnant???). I continued with my poor diet and now lack of exercise throughout the pregnancy and managed to gain 60lbs. Sitting in a reclined position is the worst thing you can do in pregnancy because it causes the pelvis floor to tighten and the uterus to tilt so the baby has to find a comfortable position somehow and mine settled ROT (right occiput transverse, right side of my stomach, back of the head towards my back and sideways, you would see the babes profile). This apparently is the best position for a baby to flip OP (occiput posterior, face up) during labor. Instead of doing that, mine just stuck his face in my pelvis. This causes a hyperextended neck and really, faces don’t dilate cervixes.
There are a number of things that I could have done differently but I’ll get to that in a bit. First I want to discuss what the optimal position is. Then I’ll tell you how to get there.
The ‘occiput anterior‘ position is ideal for birth – it means that the baby is lined up so as to fit through your pelvis as easily as possible. The baby is head down, facing your back, with his back on one side of the front of your tummy. In this position, the baby’s head is easily ‘flexed’, ie his chin tucked onto his chest, so that the smallest part of his head will be applied to the cervix first. The diameter of his head which has to fit through the pelvis is approximately 9.5 cm, and the circumference approximately 27.5cm. The position is usually ‘Left Occiput Anterior’ or LOA – occasionally the baby may be Right Occiput Anterior or ROA.
Gail Tully, creater of http://www.spinningbabies.com
is a midwife who is very knowledgable in OFP and who helped me understand my situation better, created this to help explain positioning:

SO, how to achieve optimal fetal positioning? Very simply actually. First, posture. Gail Tully and Jean Sutton say no furniture! Sit indian style in the floor, this helps open your pelvis and release your pelvic floor. Use a birth ball for better posture. “Rest Smart” Nap or sleep in positions that let your baby’s back settle in your “hammock.”
To help facilitate good positioning, pelvic tilts should be done daily and several times a day. Walking and prenatal yoga also help with positioning by moving your hips and pelvis, stretching things out and encouraging the baby to engage in an occiput anterior position. Remember though, HEAD DOWN IS NOT ENOUGH! Babies can be head down but OP (face up) or asynclitic which can cause really long hard back labors. Read here to learn more.
So you may need to figure out what position your baby is in to begin with. Belly Mapping can help with that. By feeling where the baby is, where you feel movement, where the heart beat is, the shape of moms tummy, we can figure out how the baby is positioned. It isn’t hard to do at all. Once you learn the postition, you can then focus on improving it or changing it completely. Sometimes we know before labor even starts that the baby is OP and can get the baby to rotate. There are also ways to get a breech baby to turn.
Every pregnant woman should know this information. It is so vital in ensuring that you have the best labor and delivery possible. Sometimes breech babies won’t turn and sometimes OP babies stay OP but by learning OFP techniques you are at least giving yourself a chance to make a difference.
If you are pregnant here’s a list to help with positioning:
Pelvic tilts 20 each 3x per day
Sit indian style
Do not recline
Use a birth ball
Take at least a 20 minute walk every day
Learn what position your baby is in now
Learn what to do to improve the position
Learn what to do to keep the baby in that position
Get help if you are unsure
Get help if the baby won’t move
Good luck!
EDIT: Here is some information sent to me by Ann Tumblin concerning OP babies and epidural use.
Epidural Analgesia Linked to Increased Risk of Occiput- Posterior Babies
Lieberman, E., Davidson, K., Lee-Parritz, A., & Shearer, E. (2005). Changes in fetal position during labor and their association with epidural analgesia. Obstetrics & Gynecology, 105 (5, Part 1), 974-982. [Abstract]
Summary: This prospective cohort study used periodic ultrasound examinations during labor to evaluate changes in fetal position and their relationship with epidural analgesia. The researchers sought to determine whether epidural analgesia is responsible for higher rates of fetal malposition (occiput-posterior (OP) or occiput transverse (OT)) or whether women experiencing labor with a malpositioned baby have more painful labors and are therefore more likely to request epidural pain relief. A total of 1562 nulliparous, low-risk pregnant women were enrolled in the study.
The researchers found that the position of the baby (occiput anterior (OA), OP or OT) at the time of enrollment (in the early part of active labor) predicted position at birth poorly. For instance, of the women with an OP baby at birth, only 31% had a baby in the OP position at the initial ultrasound scan. Similarly, sonograms done later in labor were also poor predictors of position at birth. The data demonstrated that changes in fetal position were common during labor, with 36% of participants having an OP baby at the time of at least one scan. More than one-half of the women who gave birth to a baby in the OP position never had an OP baby at any ultrasound assessment in labor. Overall, 79.8% of babies were born in the OA position, 8.1% were OT, and 12.2% were OP at birth.
Epidural analgesia was strongly associated with delivery from the OP position: 12.9% of women with epidurals gave birth to babies in the OP position versus 3.3% of women without epidurals (relative risk 4.0, 95% CI 1.5-10.5). Transverse position was not related to epidural use. In a statistical model that controlled for various medical and obstetric factors that could affect outcomes, epidural use was still associated with a 4-fold increase in the risk of OP birth.
The data suggest that the association between epidurals and OP babies is not because women in labor with an OP baby are more likely to request an epidural. Women who received epidurals were no more likely to have OP babies at prior to or at the time that the epidural was administered. Furthermore, women with OP babies in labor or at birth reported the same degree of pain as those with OA or OT babies and were no more likely to report “back labor,” which is commonly thought to be related to the OP position. Finally, women with OP or OT babies at birth were much more likely that those with babies in the OA position to give birth by cesarean section, with 6.3% of OA babies born by c-section versus 64.7% of OP and 73.8% of OT babies (p<.001).
Significance for Normal Birth: Epidural use increases the risk of instrumental (forceps or vacuum) delivery in first-time mothers. Experts have proposed various reasons for this association, including diminished urge to push and changes in the tone of the pelvic floor muscles that inhibit proper rotation of the fetal head. Letting the epidural “wear off” has been thought to increase the likelihood of unassisted vaginal birth, however, this systematic review calls into question that common practice.
In normal birth, there are complex hormonal shifts that help labor progress and facilitate delivery. The laboring woman produces natural endorphins that help her manage the pain of labor. Her ability to move freely and assume a variety of positions while pushing work in concert with these hormonal changes. Epidural analgesia numbs the sensations of birth, and the production of natural endorphins ceases as a result of the disruption of the hormonal feedback system. When the epidural is discontinued, the woman’s pain returns but her natural endorphins may remain diminished and therefore her pain may be greater than if the epidural had not been given in the first place. Furthermore, when an epidural is administered, the woman is usually confined to bed and attached to fetal monitors and an intravenous line. The woman and provider may become accustomed to laboring in the bed attached to machines. When the epidural is discontinued the restrictions! on her movement may persist. Under these conditions, it is likely that the impact of an epidural on normal birth may outlast the epidural itself.
EDIT: Ann Tumblin also sent me this regarding OP (face up) babies. It was done by Penny Simkin who is basically the mother of all doulas. It is very informative so if you have ever had an OP baby and are nervous about it a second time, I highly recommend you taking a look at it.


This is really interesting. I am curious, I know you mention LOA is the best, but is ROA ok? I am 99% certain my little guy is in that position, based on his butt, and where we get his heart beat. Should I try to get him to go to the left side? If so, would the suggestions you posted help with that? He has been on my right side since I could first feel him move, so maybe he just prefers that side…ha!
Amie C
June 10, 2009
ROA isn’t terrible position but it’s certainly not optimal. ROA babes have a tendency to turn OP (Face up) and you want to avoid that as much as possible. You are still relatively early in your pregnancy as far as positioning is concerned because right now you still have a lot of fluid. Lots of fluid means lots of room for baby to move still and ROA babes do move to LOA most of the time. I think that you should do whatever you can to facilitate the move especially since you are having pre labor already. Here is what Gail Tully has to say about ROA.
I am also pasting it here:
Right Occiput Anterior
ROA baby with mapI believe my baby is ROA, but you talk about the importance of the baby being LOA. You claim that LOA is the best for chin tucking and moving through the pelvic outlet.
The back of my baby is more on my right side than on my left side. There is information about exercise to turn an LOP or ROP to ROA, but not anything about ROA to LOA.
I’m not sure of the symmetry and what organs get in the way of a baby who is more to the right to keep him from tucking his chin as well, or to keep his head from fitting in the cervix as well. Can you explain more about this?
Your baby is Right Occiput Anterior.
The back is to your right, and the baby is facing towards the roomy sciatic notch in the back left of your pelvis.
This position is not clearly associated with a resulting labor pattern. The baby may rotate to the posterior and, if so, labor may have a posterior pattern of cluster contractions with slow downs or stalls. The baby may rotate to the anterior and labor may be straight forward. The main thing is whether the chin is tucked.
ROA belly map with doll
Variables with the ROA baby that effect labor;
1. Flexion of the chin
2. First time mom
3.
Balance and tone of the soft tissues relating to birthing. (This means the uterus, ligaments, and fascia.)
4. Pelvic alignment (This effects the above mentioned balance and tone.)
5. Pelvic shape and size
6. Placental location
Use the 3 Principles to give the ROA baby a chance to turn and face the back, right side and have their back on mother’s left.
1. Relax the soft tissues so that the baby can move past the placenta during labor, if the placenta is anterior or on the left.
2. Use maternal positioning to help the baby come up a centimeter and turn their head around to face the right.
Notice if there are small wiggling parts near the front, lower half of the womb. Hands in front indicate a posterior baby. The LOP baby is often labeled ROA because the forehead of the LOP baby feels the same width as the nape of the ROA baby’s neck.
Also, the weight of the baby will typically go to the bottom so if you lay on your left side then he should swing down. It may take some time but they don’t like to stay on the right because the liver is over there and it’s hard.
doulamama1
June 10, 2009
Also Amie, I had a client whose babe was ROA her entire labor. The head was also ascynclitic (meaning cocked to one side) and caused a prodromal labor (very long early labor) and radiating back labor. After a final inversion attempt in late active labor, the baby turned LOA and she went from 4cm to 10cm in an hour or so. Point is, they do turn but sometimes there are hold ups in the labor that make it much more difficult to deal with so if you can help get him to move now you may avoid some of those problems later. Laying on your left side will help the most. Do you know where your placenta is?
doulamama1
June 10, 2009
As of my last ultrasound(about 10 weeks ago) I had an anterior placenta. I may be getting another ultrasound next week due to measuring small, so I may know more then. I sleep on my left side, so hopefully that will help. I had an anterior placenta with Jordan as well, but she was on my left side pretty much my entire pregnancy(while this kid prefers the right!) I plan on getting out the exercise ball soon. I used it a lot with Jordan, mainly because my back hurt less when I sat on that, so maybe that will help too. Thank you for all this information. It is really interesting and good to know!
Amie C
June 10, 2009
An anterior placenta makes it a little more diffcult to move an ROA baby to LOA as Gail mentions in her ROA section. It can be done though. You need to really work on relaxing the soft tissues and releasing your pelvic floor. http://www.spinningbabies.com/techniques/during-labor/pelvic-floor-release
doulamama1
June 10, 2009
Aime,
I was just looking back over this post and I read your question about ROA vs LOA. Apparently Austin was ROA back when you posted this. He ended up being OP which is what I warned about with the ROA position. It is interesting that he wound up OP. I also mentioned that it is harder to get an ROA baby to LOA when the placenta is anterior but I didn’t know back then that anterior placentas result in more frequent OP babies. Being your second baby and his being so small really worked in your favor for an easy (if not super fast!) labor.
doulamama1
January 13, 2010
I was just re-reading this too, and it looks like odds where good he would be OP. I am glad it was my second and he was small. Although, I do think that the 3 weeks of timeable contractions I had was actual labor and the fast labor was all from transition on. The pain want from nothing to EXCRUTIATING. I have read that an anterior placenta is random, yet I have had it with both kids. I wonder if the odds are I will have it again if I have another kid.
Amie C
February 11, 2010
Those fast ones are TOUGH. I always say it’s called labor for a reason. Your body needs time to build up endorphins to deal with transition. When you just hit it, like you said, excruciating! I have had one client’s birth go that way and WOW is all I can say. Women always hope for a fast labor but I tell them to be careful what they wish for! I’d be curious to know if your next placenta is anterior as well.
doulamama1
February 11, 2010
I will say that I was happy it did not last long, but that pain was just unreal. I am not sure what I would want if I were to actually be given an option(because you get a choice with childbirth, right? 😉
Amie C
February 11, 2010
I’m SO glad you wrote this Amy. I’m almost positive all that bedrest between 27 and 36 weeks is what caused my malpositioning. And I’m almost positive it could have been corrected if I had known how. In case you don’t remember, my girls were both in perfect position until the 37 week ultrasound. At that point they shifted and I had both heads in my right hip, all four feet in my left rib cage and Julia’s shoulder was lodged in my cervix. I only had the weekend to get them to move before my doctor wanted to take them, as she felt that they ran a greater risk at that point of staying in than they did coming a bit early. I will most definitely be using a different OB next time. Wish more doctors would stay on top of the recent research. From what I’ve seen recently, it looks like strict bedrest often does more harm than good.
TwinMomMichelle
June 10, 2009
I haven’t read any studies discussing the risk vs benefit of strict bed rest but I would have to assume that it wouldn’t be conducive to good fetal positioning. I know there are things that can be done while on strict bed rest but I am not sure how often women are being given that information. The thing is that the body must move for the pelvis to move and for the baby to move. That stands true in both pregnancy and in labor.
Did you OB give you any suggestions to get them to move?
doulamama1
June 10, 2009
Another great post! I had an anterior placenta with my first (c-section for breech) but I didn’t know that until I read my surgical report getting ready for my VBAC. They didn’t tell me anything about placental position or fetal position except,”baby is breech” .
mamaseoul
June 10, 2009
Thanks! I was never told anything about fetal positioning either. It’s a shame really. I don’t really like to play the ‘what if’ game but had any one of the SIX doctors I saw over the course of my pregnancy had mentioned how important fetal positioning is and how much the things we do daily affect it and that we actually have the ability to change and improve it, I would have listened. Sadly, no one did and it was never discussed in my Bradley classes (which in hindsight is very surprising to me) either. I believe that this is something that should get as much attention as proper nutrition. In fact, I think OFP and nutrition should be the focus of EVERY single prenatal:)
doulamama1
June 10, 2009
Just a note – with my last baby, I had an anterior placenta, baby was incomplete breech at 40 weeks (her butt was on my left hip and her head was under my right ribs). I was attended by midwives and we did nothing but EPO by mouth to get labor started. When I went into labor at 42 weeks baby was exactly LOA. Admittedly, I did not do any OFP, but I did try a few things to just turn her from breech – ice on the top of the belly, music at the bottom of the belly, explaining to her that she was in a really bad position and she had to either get her butt down or her head (at that point I didn’t care – lol).
My point here is if we are left alone to relax and not worry about docs wanting to induce, etc., most of the time our babies will do exactly what they are supposed to do. 🙂
Jessica
June 10, 2009
Thanks for stopping by Jessica! I totally agree with you that sometimes leaving things alone is the best policy. You didn’t have the pressure or stress on you so you had less tension in your body so your baby was able to move more easily. I truly believe that there is no separation of mind and body, especially in pregnancy. I love it that you were telling her to move:)
doulamama1
June 11, 2009
I don’t know if this was asked already, but how soon should you start worrying about postion? I am at 15 wks and can’t feel the baby at this point. I do prenatal yoga and pilates and have ordered a birthing ball. Is this something I should do as early as first tri or wait til end of second into the third?
mnastasi
June 10, 2009
34 weeks for optimal birthing position but you should really start with the posturing techniques and exercises asap or no later than the beginning of the third trimester. The exercises and body prep is something that you should really do throughout the pregnancy.
doulamama1
June 11, 2009
well at least I know I am on track. I try to do the yoga and pilates 3x a week which is the same that I did for Zay. I didn’t have the ball then so I am really excited for it to get here so I can start using it and I am hoping it will help with labor as well.
mnastasi
June 11, 2009
I like this post. 🙂 A couple questions…Do you know the statistics on how many babies are malpositioned at the onset of labor? Cari was in the right position the whole time (though I’m a skeptic and didn’t know how they knew that, lol, but they were right). Do I have better chances of this baby being positioned correctly since I have had a baby already and she was in the correct position? Do you think a mother’s build has anything to do with malpositioning? And lastly, same as Mica – how soon do I need to start worrying about it?
Kate
June 10, 2009
Glad you like it Kate:) I don’t know the stats but often times they are malpositioned at the onset of labor and then turn at some point even as late as the pushing stage. I wouldn’t depend on that though because I had a client with an OP (face up) babe through out labor and her labor was a hard 36 hours long back labor. The baby did turn at the pushing stage. She only pushed three times so that was easy but the 36 hours however, was clearly not.
It is pretty easy to tell what position the baby is in, even without a clear window to the uterus;) See belly mapping
http://www.spinningbabies.com/baby-positions/belly-mapping/209-belly-mapping
and of course, the docs probably used ultrasound. I have, however, seen them tell moms that the baby is in a good position, but all they are referring to is that the baby is head down. Head down is not enough. OP is head down but not a good position. Asynclitic is head down but can cause quite a bit of added pain for mom as well. This is another one of those don’t leave it to someone else topics.
Having a baby previously does help. Gail discusses that also. Read this homepage to get an understanding of how the theory works…
http://www.spinningbabies.com/
Build can play into malpositioning but it’s more about posturing and tension and alignment. I guess all that stuff is part of ‘build’ though, isn’t it?
See my reply to Micah:)
doulamama1
June 11, 2009
Chiropractic care before and during pregnancy can help correct or prevent mal-positioning. I went to the chiropractor a few times towards the end of my pregnancy trying to get my first baby vertex and it didn’t work because I think I had a pre-existing imbalance. I tried chiropractic from 20 weeks on to turn my second breech and although it didn’t work, the version was very easy and my birthing was very easy so I do think it helps. For my next pregnancy I plan to start chiropractic before I get pregnant. Chirpractic can also help prevent or alleviate ligament pain or back pain related to the pregnancy.
mamaseoul
June 11, 2009
Yes! Great point! Alignment is extremely important to proper positioning. I need to do a bit on this too I suppose. OK Karen, you are going to have to start a list for me so I can keep up with you;)
doulamama1
June 11, 2009
Hey 🙂 I found this website on baby posistioning this morn in Mothering mag Sept/Oct 08 (special pregnancy ed.) http://www.spinningbabies.com. I have yet to check it all the way out but it looks like good info. Jessica (who is slowly working on updating her blog with her birth story!
Jessica
February 12, 2010
LOL….just scrolled up and seen someone else posted the spinning babies site! ha
Jessica
February 12, 2010
Hi jessica,
My article was based on spinning babies. If you look midway through the article at the Fetal Compass Rose, that is straight off spinning babies (as quoted above the compass). Also, many of the hyperlinks throughout the article direct the reader to spinning babies. All the spinning babies links throughout the comments section were posted by me as well. I am pretty knowledgeable about birth but I am in no way responsible for OFP techniques 🙂
doulamama1
February 13, 2010
[…] Optimal Fetal Positioning for a Better Birth […]
To Epidural or Not to Epidural « Doula Momma
June 11, 2009
[…] Optimal Fetal Positioning for a Better Birth from the DoulaMomma blog. […]
A Better Birth Through Optimal Fetal Positioning : Sweet Song Doula
June 26, 2011
[…] Optimal fetal positioning for a better birth […]
Algunas (buenas) posturas para dilatar y parir (II) | De Monitos y Risas
July 26, 2011
Here we are again, that’s Alessia and Ermanno, Francesco’s mother and father, “famous” in this website for a few posts in the PROM section in which we share our 3-week-long experience with happy ending.
Now again, Alessia is 34+6 weeks pregnant (another boy), no problems at all if not that the baby is still in breech position (podalic?) and the concern is that he might stay this way till the end. Differently from when we wrote then, we have now moved back to Palermo (Sicily – Italy) and things here are very very different from Cambridge UK! Writing about all the issues we are experiencing with NHS here in Palermo is very interesting indeed, but not for the purposes of this website, surely not in the OFP section here. However if you happen to be curious about it, just let me know, I’d be happy to unload a bit of stress with someone!
Now the questions.
1) How likely is that the baby will turn? We are quite optimistic about it, but an extra word of reassurance would be much appreciated 🙂
2) Should things stay this way, how risky is to go on with a (so longed) natural birth? Any statistics at hand anywhere?
3) What skills or knowledge are needed to the doctor who will agree to do a natural birth? Bear in mind that almost all of the breech deliveries here are made with C-Sections, so arguably they are not very experienced in that sense.
4) Should we (as we will) find resistances and no one will agree to a natural birth, how can we deal with them? IOW, they might give us “strange” reasons to justify a C-Section, how do I know they are not just pretending to make things easier for them? What knowledge do WE need?
5) What can we do to turn the baby the “right” way round? We’ve done some research about it, so we are trying a bit of everything (MOXA, “candle” and other weird positions), but the idea of having again a dedicated guide as we found it a couple of years ago in this same website (with another layout), is quite reassuring.
We hope to hear some news from you people, grazie 🙂
Ermanno, Alessia and little Francesco.
ermanno romano
September 9, 2011
[…] are very rare and that 90% of these are birthed vaginally. Please also note that my son was left mentum transverse which is considered a physically impossible position to vaginally birth. There are not many […]
Amy’s Birth Story–Inverted T cesarean for face presentation & out of hospital VBASSC | ICAN Blog
February 8, 2012
[…] Reprinted with permission from Doula Momma’s site. Original link can be found here. […]
Optimal Fetal Positioning | ICAN Blog
February 13, 2012
I have three children, the first born in hospital, 4 hour labour no complcations very positive experience, the second, water birth at home
1 1/2 hours beautiful experience. The third, water birth at home ,under an hour,too fast to enjoy.
I thank wonderful midwives , yoga and bellydancing. All of these helped me to have a deeper sense of awareness in my body and to also trust in myself to be able to birth in a good way. Teaching bellydancing and pregnancy yoga, it amazes me how few women take this path to a wonderful pregnacy and birth.
Melissa.
Melissa Arnott-Barker
February 13, 2012
Hi I found this very interesting. I’m 38w6d pregnant and my baby just turned from LOA to OP 😦 She was LOA for weeks and weeks then I was on the bus on my way to a Midwife appointment and she suddenly turned. It’s very uncomfortable having her in this position and I’m so worried about labour now that she’s suddenly moved. I didn’t know about OFP until today, which makes me sad and concerned it’s much to late to do anything as I didn’t know about all the exercises I should be doing.
I’m not sure what to do to get her to move back to LOA. A lot of your links don’t work anymore btw but I did go right to the spinningbabies website but I found all the information overwhelming. Please help me get this baby back into the right position!
Brianne
July 19, 2012
Hi, did you hear back on this? How did things go for you. My babe moved to ROT at exactly 39 weeks! I have days, if that, to sort it out.
Carrie
August 21, 2015
[…] circumstances and decisions – i.e. when your water breaks, pitocin and labor induction, position of the baby, […]
The Overwhelming Resource for “All Things Baby” (Part 1) | Shesourceful
September 10, 2012
[…] I have a much better handle on my blood sugar issues, I’ve been spending more time thinking about optimum fetal positioning. With about eight weeks to go, I still have time to help encourage this kid to be in good […]
Great Expectations: Pamela @ 32 weeks — Giving Birth with Confidence
October 26, 2012
[…] for Normal Birth. 2. Lamaze International, teaching handout Photo 1 Thunder Bear and Wren Photo 2 Doula Momma Photo 3 Blessed […]
Understanding “Labor Lingo”
November 28, 2012
[…] https://doulamomma.wordpress.com/2009/06/10/optimal-fetal-positioning-for-a-better-birth/ […]
Apresentações do Bebê | Bibliografia da Doula
May 4, 2013
Way cool! Some very valid points! I appreciate you penning this article and the
rest of the site is also very good.
more on music documenting faculty
July 13, 2013
Excellent post. I certainly love this site. Keep it up!
visit Music recording college
July 13, 2013
If you desire to obtain much from this post then you have to apply these techniques to
your won blog.
my baby freebies
August 4, 2013
[…] my right side, but that he was face up, Right Occiput Posterior (ROP), instead of facedown. The best birthing position for any baby is Occiput Anterior (OA), which is facedown, facing your back. This position is best […]
LIFE: Our Home Birth Story: 42 weeks + 5 Days – Bringing Design Home
August 8, 2013
Attractive element of content. I just stumbled upon your
site and in accession capital to claim that I acquire
actually enjoyed account your blog posts.
Anyway I’ll be subscribing to your augment and even I achievement you get entry to
persistently fast.
health and welbeing - measurablemarketingstrategy.com
September 1, 2013
Thank you for this information and sharing your personal story. Do you have suggestions for sleeping positions? I am at 28 weeks and will try to figure out the position my baby is in. Part of me thinks transverse with bottom to the left and head to the right. But I am not sure.
Meli
September 3, 2013
[…] útero. Em vários casos de mal posicionamento do bebê ele pode ser usado. Até mais! Fonte: https://doulamomma.wordpress.com/2009/06/10/optimal-fetal-positioning-for-a-better-birth/ http://www.babyzone.com/pregnancy/position-of-baby/delivery-baby-position_70441 […]
Apresentações do bebê » Doulas Londrina
May 11, 2014
Reblogged this on Love gentle birth and commented:
Wonderful suggestions and information about helping baby get into and stay in an optimal position for labor and birth.
lovegentlebirth
July 1, 2014
I know you posted this a long time ago, but just wanted to say it’s the first time I’ve ever seen a photo that clearly shows what my son’s position would have been when I had him (LMP) in 2008….. Thanks for including the ‘rare’ positions for people whose babies are not in one of the ‘normal’ spinning babies positions!
Nicole
September 30, 2014
hi
im 31 weeks with roa . plz suggest what to do for natural birth;
suk
June 17, 2016